The Unofficial Guide to Paediatrics is unique in that it is the only textbook that covers core subject summaries, examination practice, practical skills, career opportunities and clinical cases all in one place. It does this through 1000+ colour images and illustrations, 200+ multiple choice questions, and 60+ real life clinical cases to bring paediatrics to life. The contributors range from Professors of Paediatrics, to medical students, to teachers, nurses, and midwives, meaning the book has influences from a truly multidisciplinary team at all stages of training.
Almost every doctor will encounter children in their career; of course, this goes without saying for paediatricians, and in primary care approximately 25% of consultations involve children. Many other specialities encompass paediatric patients including general surgery, ENT and emergency medicine. Therefore, it is vital that all medical students and junior doctors have a core grounding in the fundamentals of paediatrics.
This book is primarily aimed at medical students, covering a wide range of common and important paediatric pathologies (in line with the national Royal College of Paediatrics and Child Health undergraduate curriculum). The unique collection of core clinical content, practical skills, clinical cases and examination skills in the book is equally valuable for junior doctors and paediatric trainees. Nurses, advanced nurse practitioners, physician associates and allied healthcare professionals will also find the content and approach useful.
The relevance of this book extends from undergraduate teaching to postgraduate education and as a day-to-day reference for healthcare professionals.
Key Features
Written in line with the other books in the series, stations contain:
Core chapter summaries written using the latest guidelines, using a clinically relevant format for maximum knowledge and minimum waffle
Single best answer, true or false and extended matching questions to enable you to really test your knowledge.
Over 300 questions and fully explained answers with key points and compact learning summaries.
High quality colour images and illustrations throughout the book to present key concepts and anatomy.
Core Topics
24 fully illustrated chapters cover the core fundamental knowledge base of paediatrics, in line with the national RCPCH curriculum. Each disease uses a common framework; definition, aetiology and clinical features, and progresses through investigations, differential diagnoses, management, complications, and finally prognosis.
- ADOLESCENT MEDICINE
- ASSESSMENT AND MANAGEMENT OF THE ACUTELY UNWELL CHILD
- CARDIOLOGY
- COMMUNITY PAEDIATRICS
- ENT
- ENDOCRINOLOGY
- GASTROENTEROLOGY
- GENETICS
- HAEMATOLOGY
- IMMUNOLOGY AND ALLERGY
- INFECTION
- INTENSIVE CARE
- CHILDREN AND THE LAW
- METABOLIC MEDICINE
- NEONATOLOGY
- NEUROLOGY
- NUTRITION
- ONCOLOGY
- ORTHOPAEDIC AND RHEUMATOLOGICAL DISORDERS
- PUBLIC HEALTH
- RENAL MEDICINE
- RESPIRATORY MEDICINE
- SKIN CONDITIONS
- SURGERY

Zeshan Qureshi
Chief Editor
Paediatrics trainee at Great Ormond Street, and the Institute of Child Health
Thank you for taking a look at this book. It sums up what I would have wanted to know to get through Paediatrics.
With over a 1000 illustrations, 60+ clinical cases, 200+ MCQs, examination routines, practical skills, walk through OSCE scenarios, it is truly a unique book that teaches Paediatrics in way that caters to everyone’s needs, with a lot of fun to be had along the way!
This section aims to help those transitioning to clinical paediatrics, either on placement, or working as a doctor. History taking, examination, practical skills and communication skills are all described, again in the context of real-life clinical cases, bringing the theory to life. Examination and practical skills are fully illustrated with professional child actors to give absolute, step-by-step clarity.
69 clinical cases, divided into standard, intermediate, and difficult allow the reader to apply the knowledge gained through the core topics to real life scenarios. All cases have full explanations to the answers, detailing not just why the ‘correct’ answer is ‘correct’, but also why ‘incorrect’ answers are wrong, leaving the reader in no doubt about the reasoning behind the answer. Important learning points from every clinical case and key points from each individual question are also highlighted.
A step-by-step guide to a real life case
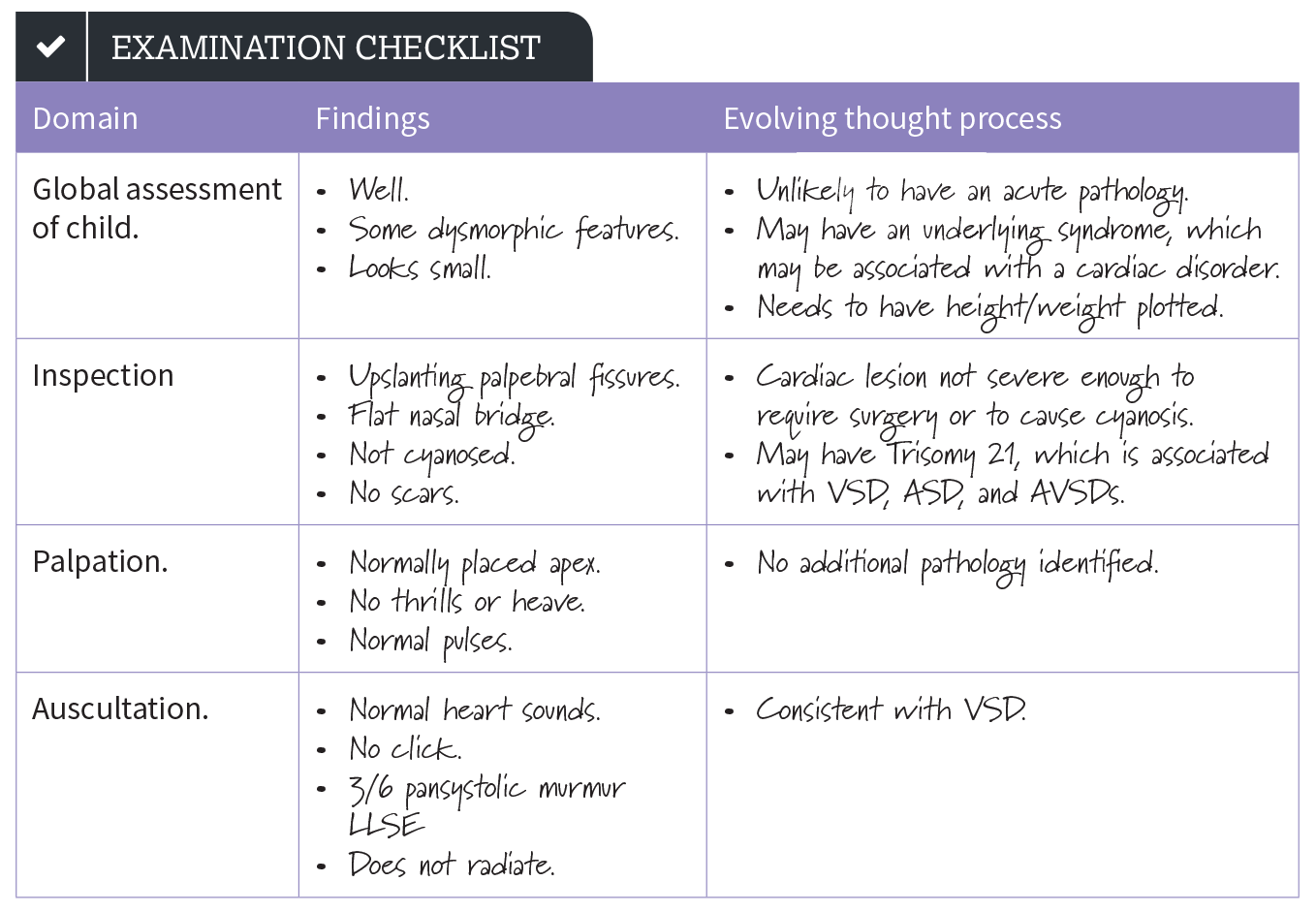
Thomas is a six-year-old boy who has attended clinic today for review of his murmur. You have been asked to perform a cardiovascular examination on him and present your findings.
Exactly what to say when presenting your findings so that the examiner or your senior doctor knows exactly what you are talking about!
Thomas looks well and appears comfortable and acyanotic at rest. He has dysmorphic facies, with upslanting palpebral fissures and a wide flat nasal bridge.
Thomas has a normal pulse rhythm and volume with a rate of 92 beats per minute. He has no scars on his chest.
His apex beat is non-displaced. On auscultation of his chest, he has a 3/6 pansystolic murmur heard loudest at the lower left sternal edge that does not radiate. There is no evidence of cardiac failure.
These findings are consistent with a VSD in a child with Trisomy 21. To complete my examination, I would like to plot Thomas’ height and weight on an age and sex, trisomy 21 appropriate growth chart, measure his BP and perform an ECG. To confirm the diagnosis of a VSD, Thomas would need to be referred for an echocardiogram.”
TW: Contains description of self-harm
A 14-year-old girl presenting with self harm
Jennifer, a 14-year-old girl, is brought in by her mum after having self-harmed by cutting her arm with a razor. On assessment, the cuts are shallow and horizontal, with no active bleeding. The girl is quiet and withdrawn, but appears otherwise well. This is her first episode of self-harm. When asked whether she wanted to kill herself, she shrugs. Observations are within normal limits.
After being reassured that her cuts do not require further treatment, both Jennifer and her mother are keen to go home.
You are then asked the questions that Paediatricians have to think about every day…..
- Which of the following would be the best way to manage Jennifer?
- Jennifer should be sectioned because she is suicidal
- She should be discharged home in her mother’s care, because she is a child
- She should be assessed before discharge by the child and adolescent mental health team, either in the ED or as an inpatient
- She should be discharged on her own because she has been assessed as Gillick competent
- Jennifer should be sectioned because she is suicidal – Incorrect. Although this is a possibility, it would be very rare to need to section a patient following self-harm. This patient appears to be cooperative and not an immediate risk to her own safety, so there are other options that are more appropriate.
- She should be discharged home in her mother’s care because she is a child – Incorrect. Children and young people should generally be admitted following a significant episode of self-harm. This could be admission to a paediatric or adolescent ward, if available. In some circumstances, review by the mental health team may occur in the ED, and if a plan is put in place for a safe discharge, this can be followed, but it is not the norm.
- She should be assessed before discharge by the child and adolescent mental health team, either in the ED or as an inpatient – Correct. Usually patients are only discharged from the ward after being formally assessed by child and adolescent mental health services. This may happen in the ED, depending on when the young person attends. If an assessment is not available on the same day, she should be admitted until she is assessed. It is also important to consider child protection concerns, and it may be appropriate to inform social care.
- She should be discharged on her own because she has been assessed as Gillick competent – Incorrect. As above, she should be admitted. Irrespective of her Gillick competence, she cannot refuse treatment that is deemed in her best interests.
Key Point
Ensure all children presenting to hospital with self-harm have a formal specialist assessment of their risk of suicide before discharge.
This final section focuses on understanding the core requirements of paediatric assessments (including OSCEs) and jobs. It also covers life as a paediatric junior doctor and career opportunities, empowering the reader to progress from a student in paediatrics, to working in paediatrics, and finally to their final paediatric sub-specialty interest.
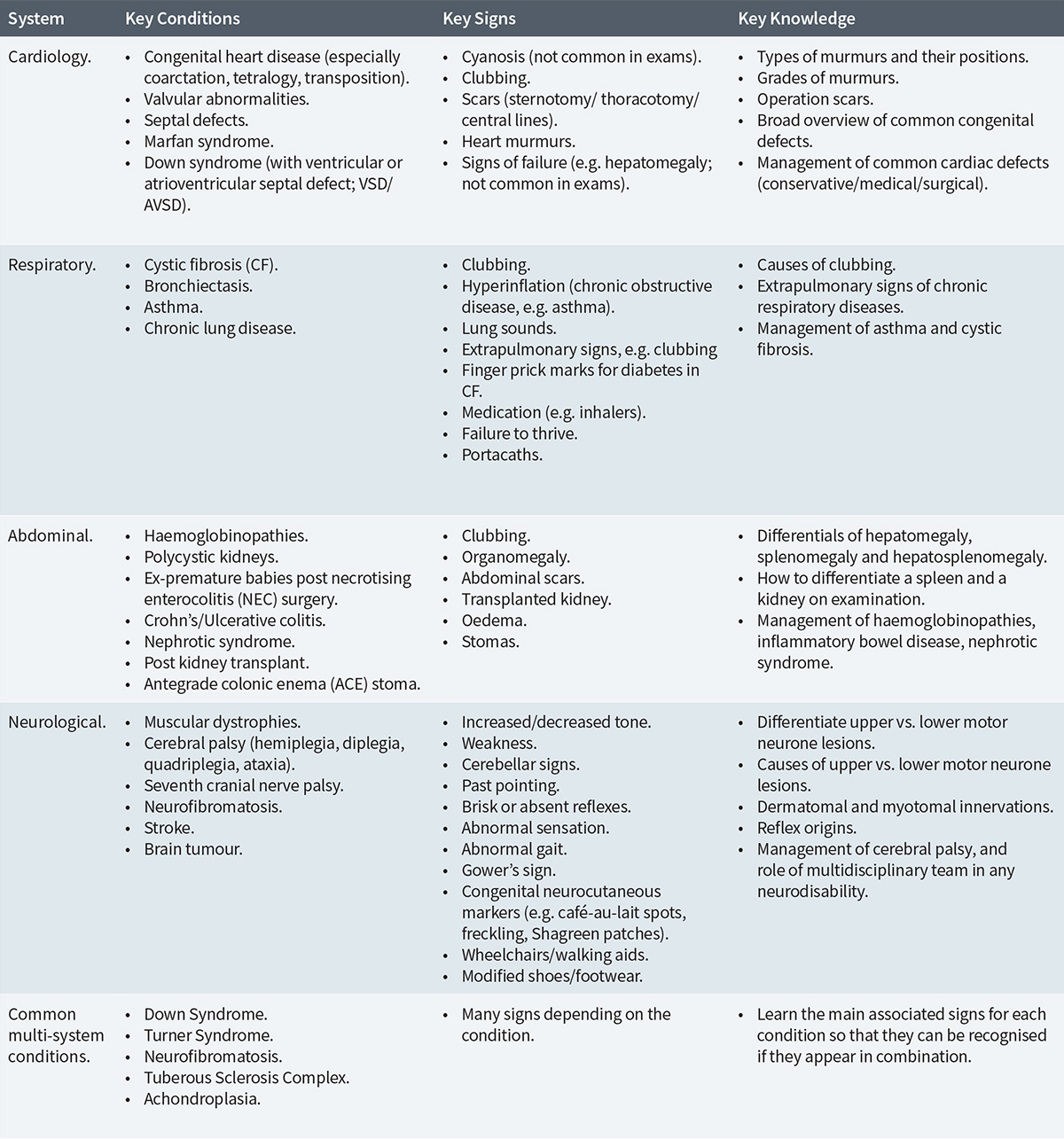
We tell you what you need to learn for OSCEs
Common Examination Findings in Paediatric Exams and Common Underlying Diagnoses
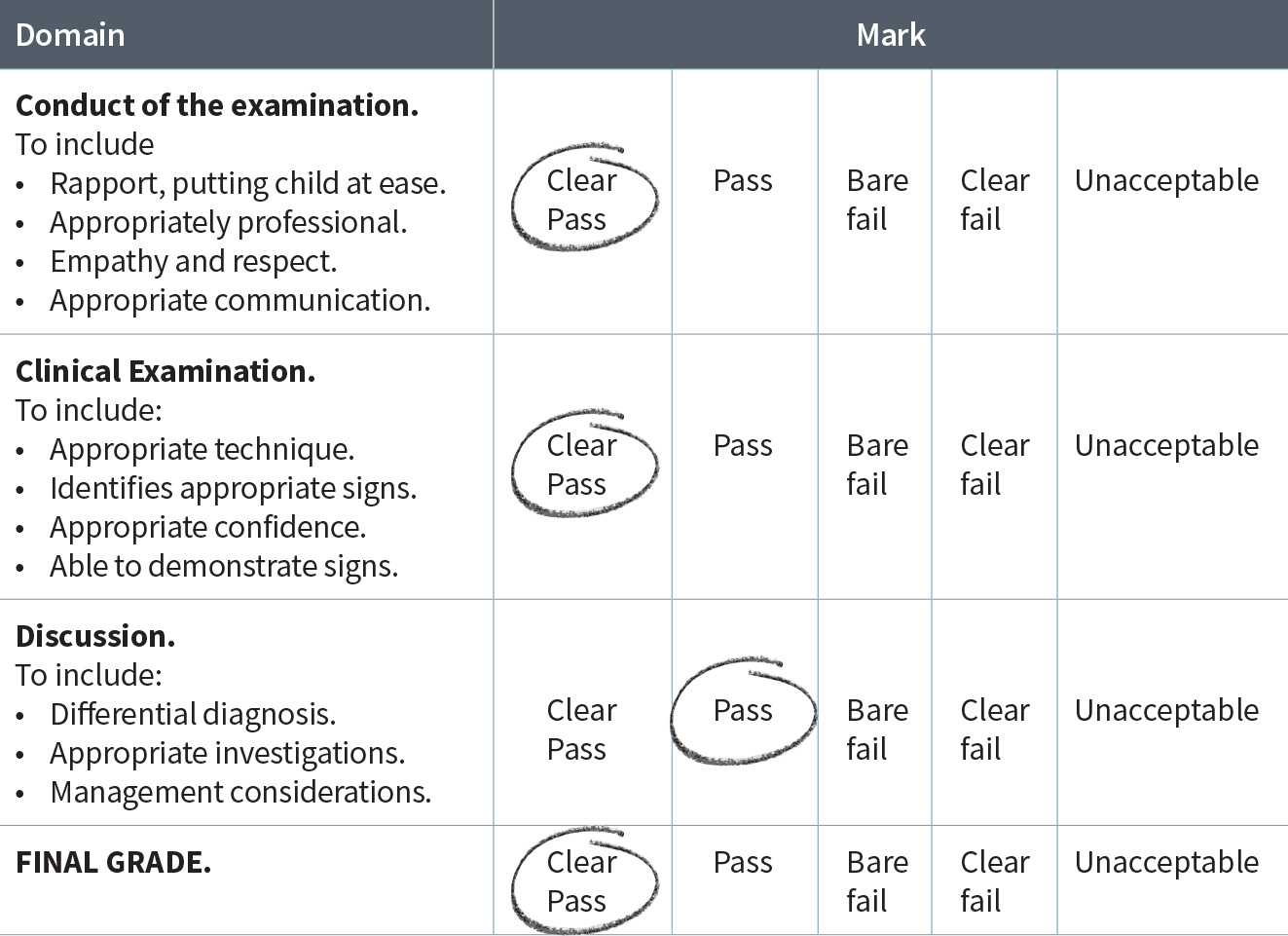
Examination Mark Scheme
Contact Us
Are you a medical trainee, a student, a doctor or medical professional?
We’d love to hear from you for feedback or if you would like to contribute towards the Unoffical Guide to Medicine series.