The Unofficial Guide to Prescribing lays out the practical steps of how to assess, investigate and manage a patient, with a focus on what to prescribe and how to prescribe it. Its aim is to empower newly graduated junior doctors to excel at dealing with emergencies and handling complex prescribing scenarios.
Prescribing errors cost healthcare systems millions annually, so early training in prescribing has become an urgent priority of medical education and now forms an essential part of teaching and assessment. The Unofficial Guide to Prescribing is a new book designed to address this requirement. It is written by junior doctors still close to the transition from theory to practice, overseen by a review panel of senior clinicians to ensure accuracy, and designed to help medical students practise and learn as much as possible about prescribing, in actual clinical scenarios, before they have to do it for real.
Prescribing is a major challenge for students because of its volume and complexity, and the need to gather experience.
It is the thing that new graduates fear the most and feel least prepared for, and it’s the commonest thing new graduates do which directly affects patient safety and can produce clinical errors.
Key Features
Each scenario is broken down into the following:

Zeshan Qureshi
BM BSc(Hons) MSc
Co-editor
Paediatrics trainee at Great Ormond Street, and the Institute of Child Health
The Unofficial Guide to Prescribing is designed to take the theoretical knowledge of medical school and apply it to real life practical situations.When a 55-year-old man with a new diagnosis of Hodgkin lymphoma is confused with a sodium of 118, what do you do?
When a 17-yearold girl is unresponsive with a blood sugar of 1.8, what do you do?
Much like its OSCE companion, this book will take you through the practical steps of how you assess, investigate and manage each individual patient, with a focus on prescribing, specifically what you prescribe, and how you prescribe it; with clear examples of generic drug charts showing you how the prescriptions would look in real life.
Station 8.2: Acute Pancreatitis
You are the surgical junior doctor in the emergency department. A 42-year-old obese female with a background of gallstones presents with severe epigastric pain radiating to the back. She has vomited on multiple occasions and feels that she is becoming more breathless. Please assess her and commence appropriate management.
Patient Details
| Name: | Jane Smith |
| DOB: | 05/03/72 |
| Hospital Number: | J35789 |
| Weight: | 85kg |
| Height: | 1.6m |
| Consultant: | Mr King |
| Hospital Ward: | BFH Surgical |
| Current Medications: | None |
| Allergies: | No known drug allergies |
| Admission Date: | 22/09/14 |
Initial Assessment
AIRWAY
Assess the patency of her airway. Does she have any vomitus obstructing her airway?
‘The airway is secure and patent, as she is responding to questions.’
Continue to monitor the airway, but no intervention currently required.
Breathing
Assess the rate and depth of respiration. Is she using her accessory muscles for respiration? Check oxygen saturations. Auscultate her chest: does she have any degree of lung impairment, crackles or wheeze?
‘RR 28/min, oxygen saturations are 92% pre-oxygen therapy. She is using her accessory muscles of respiration. She has reduced air entry and crackles are heard throughout both lung fields bilaterally with some wheeze. She is complaining that she cannot catch her breath.’
This lady is tachypnoeic and unable to maintain normal saturations. She requires highflow oxygen on a non-rebreather mask, and optimization of pain control. Could consider NSAIDs or other opiates such as pethidine or tramadol, but trial morphine if pain is severe: a PCA may be required to control the pain.
Circulation
Assess her CRT, pulse and blood pressure. Check her mucous membranes and assess her hydration status by looking at her tongue and skin turgor.
‘HR 115 bpm, BP 90/60 mmHg, and CRT 3 seconds peripherally. Her hands are moist and cool with a thready pulse. Her mucous membranes are dry. Her eyes appear sunken. Her heart sounds are normal with no murmurs.’
This lady is intravascularly depleted. She needs aggressive fluid resuscitation. Two large bore IV cannulae (14 or 16 G) should be inserted (while simultaneously taking bloods) and a fluid challenge should be given (e.g. over 15 minutes). A urinary catheter should be inserted to assess end-organ perfusion.
Differential diagnosis of epigastric pain
- Inferior MI
- Peptic ulcer disease
- Perforated peptic ulcer
- Symptomatic gallstones
- Dissecting aortic aneurysm
- Small bowel obstruction
- Oesophagitis
Causes of acute pancreatitis
- Gallstones (40%)
- Alcohol (40%)
- Idiopathic (10%)
- ERCP
- Hyperlipidaemia
- Viral (mumps, coxsackie)
- Drugs (azathioprine, tamoxifen, corticosteroids, valproate, ASA)
- Autoimmune (vasculitides)
Complications of pancreatitis
- Early: shock, acute respiratory distress syndrome (ARDS), SIRS, hypocalcaemia, renal failure, hyperglycaemia, retroperitoneal haemorrhage
- Late: pseudocyst formation, pancreatic abscess formation, necrotizing pancreatitis, recurrent pancreatitis, pancreatic cancer
Management Summary: Acute pancreatitis
- Aggressive resuscitation
- Assessment of disease severity
- Early ITU involvement in severe pancreatitis
- Imaging to identify aetiology and severity
- Early nutritional support
- Avoid antibiotics unless disease identified
- Treatment in specific aetiology (i.e. ERCP)
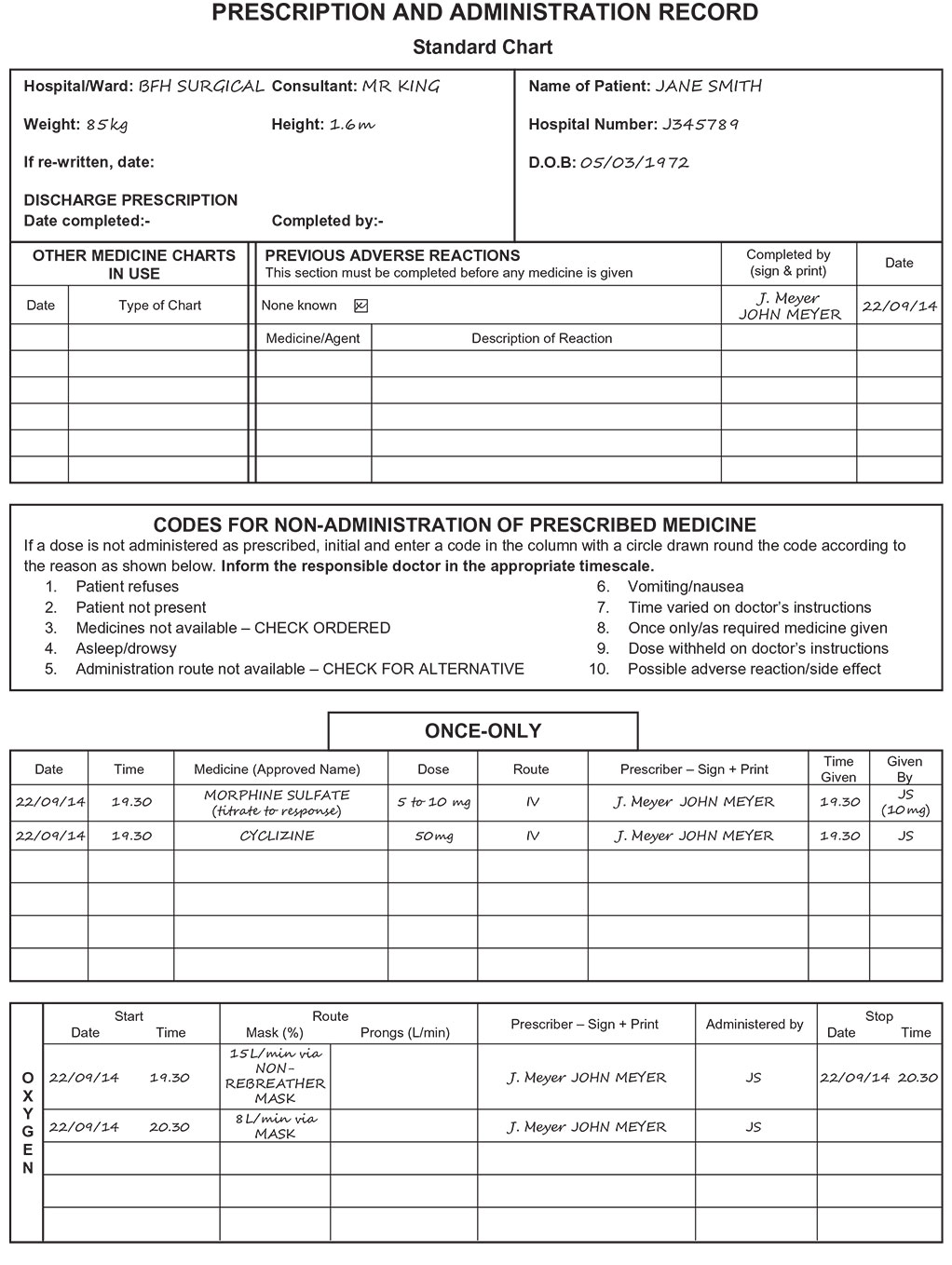
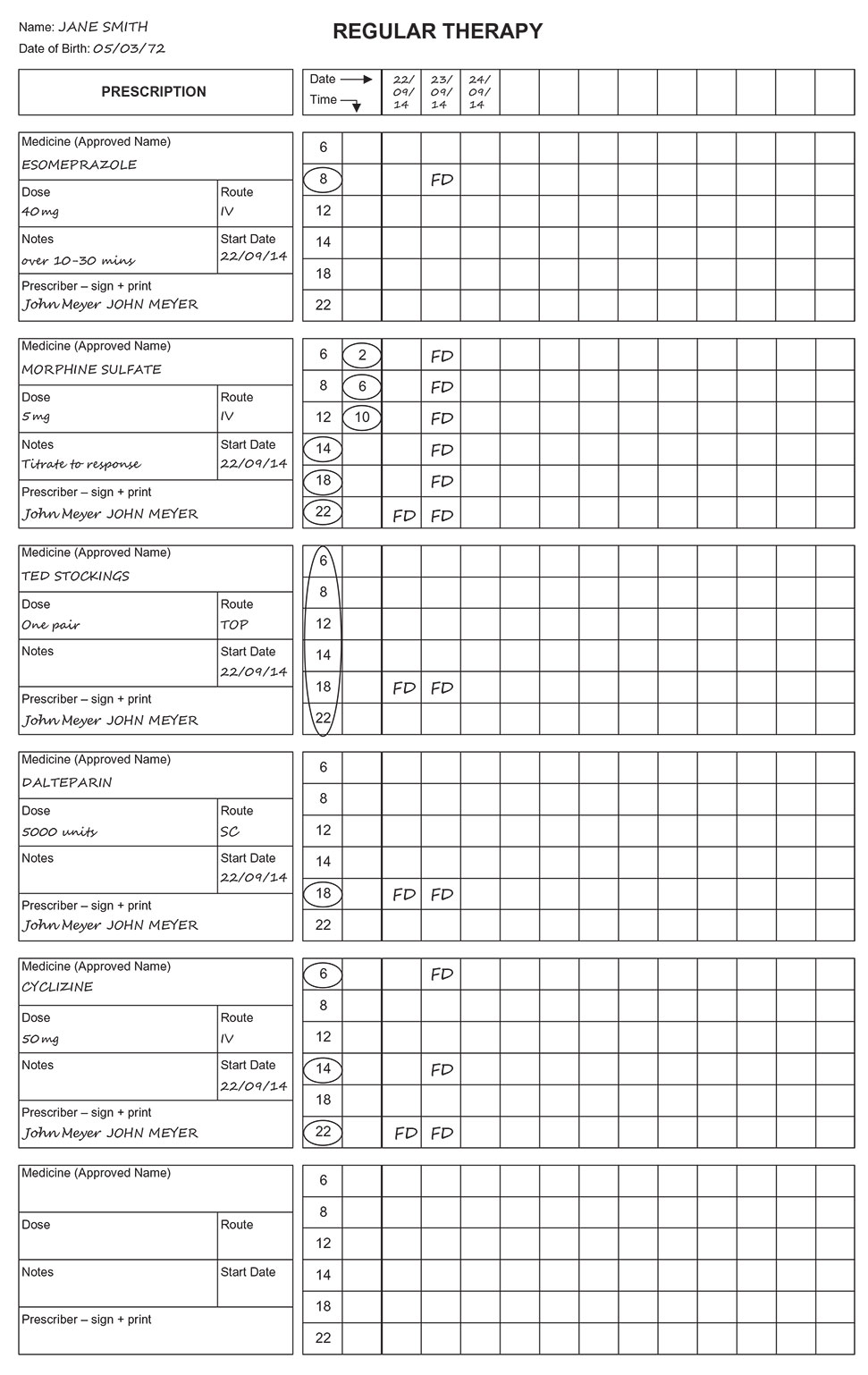
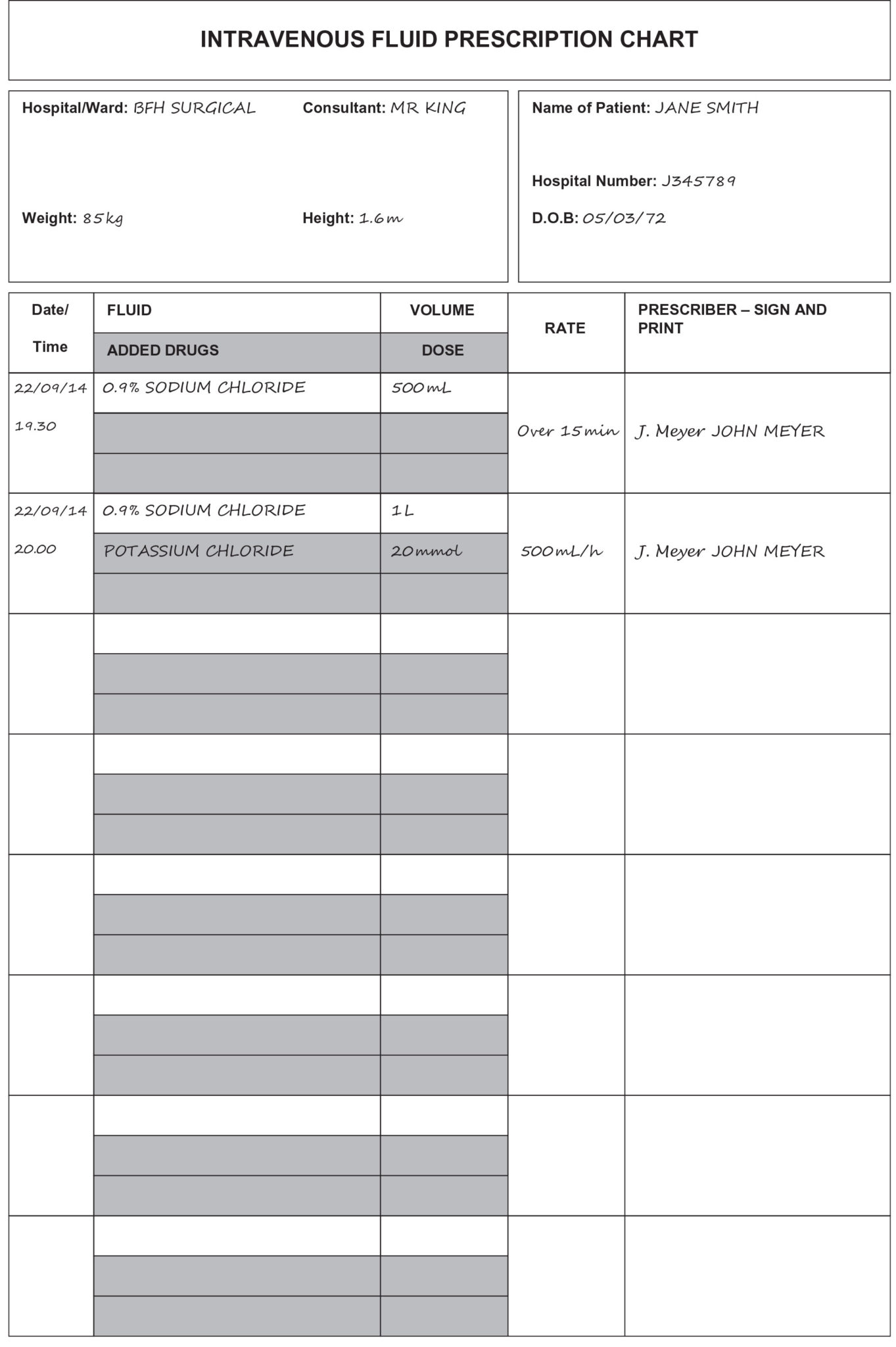
Administration and Prescription Charts
Prescribe
High-flow oxygen: 15 L/min OXYGEN via NON-REBREATHER MASK Analgesia, e.g. MORPHINE SULFATE 5 to 10 mg IV (titrate to response)
CYCLIZINE 50 mg IV STAT (to reduce morphine-related vomiting) Fluid bolus, e.g. 0.9% SODIUM CHLORIDE 500 mL IV (over 15 min)
Prescribe
Proton pump inhibitor, e.g. ESOMEPRAZOLE 40 mg IV (over 10–30 mins) OD
Thromboprophylaxis, e.g. DALTEPARIN 5000 units OD SC and TED STOCKINGS TOP CONT
Regular analgesia, e.g. MORPHINE SULFATE 5 mg 4 HOURLY (titrate to response) IV (with antiemetic, e.g. CYCLIZINE 50 mg IV TDS)
Prescribe
Further fluids, e.g. 0.9% SODIUM CHLORIDE 1 L with 20 mmol KCL 500 mL/h
OXYGEN, e.g. 8 L/min via MASK
STOP
Initial oxygen prescription
Contact Us
Are you a medical trainee, a student, a doctor or medical professional?
We’d love to hear from you for feedback or if you would like to contribute towards the Unoffical Guide to Medicine series.